The birth control pill has been called the most important scientific advance of the 20th century, and no wonder. Fifty years after its approval by the Food and Drug Administration, it is still one of the leading methods of contraception, in the United States and around the world.
Much has been written about how it revolutionized sexual and social relationships, allowing women to defer pregnancy, enter the work force and make life choices their mothers could not — or, if you prefer, spawning promiscuity and undermining the foundations of marriage.
But the pill also led to profound changes in the F.D.A. itself — a revolution in what Dr. Margaret Hamburg, the current food and drug commissioner, calls regulatory science. Many of the steps that underlie modern drug approvals — extensive clinical trials, routine referrals to panels of outside experts, continuing assessments of a medicine's safety, and direct communications between the F.D.A. and patients — were pioneered to deal with evolving concerns about the pill's safety.
In regulatory terms, the pill brought about a kind of reformation: just as Martin Luther insisted that individual Christians could communicate directly with God without the mediation of priests, the pill eventually led the F.D.A. to communicate directly with patients without going through doctors.
That change, fiercely resisted by some physician groups, is now firmly entrenched; the F.D.A. now routinely requires that many medicines carry significant and sometimes complex warnings that patients are expected to read and understand.
But the pill was the first.
"The F.D.A. had been battling with the American Medical Association for years about who would talk to patients," said Daniel P. Carpenter, a professor of government at Harvard. "And with the pill, the F.D.A. clearly established the upper hand."
The pill's role in the maturing of the F.D.A. has often been overlooked because shortly after the agency's approval of the contraceptive, news of the horrific effects of thalidomide swept the world. That drug had been introduced in Europe as a sedative but was withdrawn in 1961 after it was linked with profound birth defects.
Although thalidomide was never approved in the United States, the horror surrounding its effects led Congress to toughen the drug approval process by requiring manufacturers to prove their medicines were both safe and effective.
It was a standard the F.D.A. had already been putting into effect, quietly if fitfully, in part because of the growing view that the safety of a medicine was inextricably linked with its efficacy.
Enovid, a pill combining the hormones estrogen and progestin, was already being prescribed for menstrual problems. But in approving it as a contraceptive, the agency's reviewers required Searle to prove that it was effective in preventing pregnancy. (If it worked, the pill would spare women the risks of pregnancy and childbirth, which dwarfed any known risks from the drug.)
So the company undertook one of the most extensive clinical trial programs to date, said Suzanne Junod, an F.D.A. historian. The pill was formally tested in 897 women, mostly in Puerto Rico and Haiti.
The trials were relatively brief and did not answer fundamental questions about risks of cancer, heart disease and other chronic diseases. Uncertain about the long-term effects of hormonal contraceptives, the F.D.A. mandated that doctors limit prescriptions to two years.
The pill's overwhelming popularity, however, soon rendered this limitation unenforceable. New versions were introduced, so women could simply switch brands — or find another doctor to prescribe the old one. And many doctors ignored the limit anyway.
Then in November 1961, a British physician reported in The Lancet that a young woman had developed a blood clot and died while taking the pill. Within months, two similar fatalities were reported in the United States, and by August 1962, the F.D.A. had received 26 reports of users' suffering blood clots.
By the end of 1964, more than four million women had used Searle's pill, and a blizzard of competitors had begun to blanket the market. With something so popular, the agency had no way of knowing if the problems experienced by users were related to the pill or would have happened anyway — the kind of mystery that has plagued drug regulators ever since.
So agency officials did two things for the first time that would eventually become routine. They asked a panel of outside experts to review the evidence on a continuing basis, and they and British regulators pressed for a large epidemiological investigation that would become a model for the future.
Even before the pill, the federal government had a long history of using advisory committees to assess specific subjects and issue reports. But in 1965, the F.D.A. established its first permanent advisory panel, the Obstetrics and Gynecology Advisory Committee, largely to track the safety of the pill. The agency now has 32 permanent advisory committees, one of them with 18 different panels. These committees provide crucial advice not only about whether to approve certain medicines and devices but also how to address safety concerns that arise after approval.
"What the pill does," said Dr. Carpenter, of Harvard, "is show the F.D.A. that postmarketing surveillance is a tough problem."
The challenge of communicating these risks to patients while still supporting the product's continued use bedeviled top agency officials. Protests by women's groups and hearings on Capitol Hill made clear that despite the agency's attempts, many women said they took the pill without being fully informed of its risks.
Frustrated that some doctors were not communicating adequately with their patients, the F.D.A. created a handout in 1975 that doctors could use in counseling patients. Many doctors, incensed at what they saw as the agency's intrusion into the doctor-patient relationship, either ignored the material or refused to give it out.
In 1978, faced with mounting complaints that women did not have the information they needed, the F.D.A. mandated that patients be given the handouts when they picked up their prescriptions at the drugstore.
"It was the first time that the agency had provided information directly to patients at the point of sale instead of relying on physicians," said Dr. Junod, the historian.
More recently, the Ortho Evra birth control patch has become a telling example of the continuing challenges that the F.D.A. faces in regulating a global, multibillion-dollar industry on which the agency depends for crucial information about drug safety.
Johnson & Johnson developed the patch in hopes of exposing women to even lower doses of estrogen than they got with the pill. But the company's own studies showed that the patch actually delivered far higher doses.
The finding was buried in a mathematical formula in a 435-page report filed with the F.D.A. The company said it acted responsibly, but after four years, the F.D.A. issued a warning about high estrogen doses, and sales plunged.
One last bit of lore about the pill: no one is even sure when to celebrate its birthday. Ten years ago, the agency honored the occasion on June 23, the date that the F.D.A. gave formal approval for Searle to market the product. This year, the agency is celebrating on May 9, which coincides with the period 50 years ago when it announced its intention to approve the pill when a few technical details were ironed out. That this happens to be Mother's Day this year may have played a role in the decision.
But whatever the date, it represents the F.D.A.'s first steps into adulthood.
"The pill was a landmark in the field of drug regulation," said Peter Barton Hutt, a former top agency lawyer. "This is the drug that started it all."

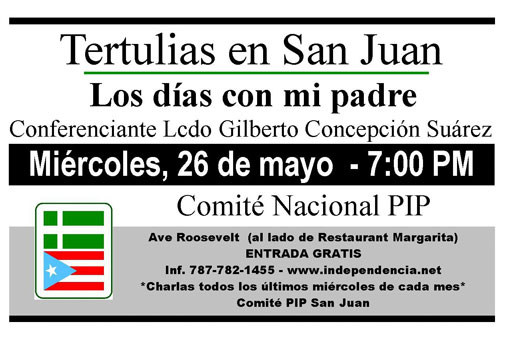

 Estamos en el siglo 21 y a esta altura de la historia Puerto Rico es una colonia de los Estados Unidos.
Estamos en el siglo 21 y a esta altura de la historia Puerto Rico es una colonia de los Estados Unidos. 






